COVID-19 Guidelines (intranet link to look for most updated PDF) and look for “Mount Sinai Preprocedure COVID-19 PCR Testing Guidelines PDF (updated June 11, 2020)” and “COVID-19 Pre-Testing FAQ PDF” (updated June 10, 2020)
As of June 9, 2020, NYC Health has recommended that all New Yorkers get tested, regardless of symptoms.
Patient Testing - Asymptomatic Patients
Who to test
- Testing capacity may vary depending on the clinical site and/or unit you are operating in. Please communicate with your medical team about testing asymptomatic patients at that site
- Generally speaking, NYC.gov recommends that all New Yorkers should be tested. This varies from NY State guidelines which recommend only asymptomatic individuals that meet certain criteria (essential/phase 1 workers, exposure to COVID-19+ patients, protestors, etc.) get tested
Where to test
- Please consult with your team for onsite testing of asymptomatic patients as these practices may vary by clinical site/unit
- Direct NYC (5 boroughs) residents to the NYC.gov COVID-19 website to find the nearest testing site
- Direct NY residents not from NYC to the NY Department of Health website to see if they meet testing criteria and find the nearest testing site
Patient Testing - Symptomatic Patients
Who to test
- NY guidelines recommend that all symptomatic patients be tested (symptoms include fever or chills, cough, shortness of breath, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion/runny nose, diarrhea)
- If a patient is exhibiting symptoms, please inform your team AND triple check the patient’s chart for COVID-19 testing status
- Reminder: Always check the patient’s chart for COVID-19 status using a computer, iPad mini provided by MedEd or other mobile device PRIOR to entering the patient’s room
Where to test
- Please consult with your team for onsite testing of patients as these practices may vary by clinical site/unit.
- Patients can use the NY Department of Health website to find the nearest testing site
Red flags
- Emergency warning signs - trouble breathing, persistent pressure and/or pain in the chest, new confusion, inability to wake or stay awake, bluish lips or face.
- A negative result in symptomatic patients who are not improving is high suspicion for false negative test results.
- Consider reaching out to Infection Prevention and continuing isolation
Patient Testing - Pre-Procedural Testing
Who to test
-
Patients undergoing procedures in the main operating room and major procedural areas (cardiac catheterization, interventional radiology, electrophysiology, and endoscopy areas), Ob/Gyn procedures, as well as any procedural areas that require at least moderate sedation will be tested for COVID-19 optimally 2 days, but no more than 3 days before the scheduled procedure.
- Exception: The patient has a previously positive COVID-19 PCR test result with resolution of symptoms.
What if a patient tests positive?
- Procedures should NOT be performed in patients with a new positive COVID-19 PCR test or active symptoms UNLESS the procedure is emergent or there is absolute medical need to proceed.
- If a patient has a prior positive COVID-19 PCR test with or without symptoms, delay the procedure until > 14 days have passed since the PCR test AND the patient has been afebrile (temp < 100F) for 3 days (without antipyretics) and has had significant resolution of respiratory symptoms.
Reminder: These are general guidelines. Specific protocols may vary by site. Always consult your team for site-specific information.
Click HERE (intranet link to look for most updated PDF) under “Mount Sinai Health System Operating Room Guidance for PUI” updated 3/26/20 for information on operating on a COVID-19 positive patient
Student Testing
- Currently, there are no plans for regular testing of asymptomatic students
- If you are concerned about a high-risk exposure or are symptomatic, please contact your PCP or student health about the appropriateness of testing. Please see the “If You Feel Sick With COVID Symptoms” section for more information
- All students are encouraged to take advantage of free antibody testing available to all Mount Sinai employees
Antibody testing
(See link HERE for updated PDF see FAQ for Antibody Testing PDF):
Serological assays are important for convalescent plasma therapy practices to support the immunity of COVID-19 patients. MSHS is participating in the FDA Convalescent Plasma Expanded Access Program (EAP), sponsored by the Mayo Clinic and overseen by the Mayo IRB.
What is the antibody test?
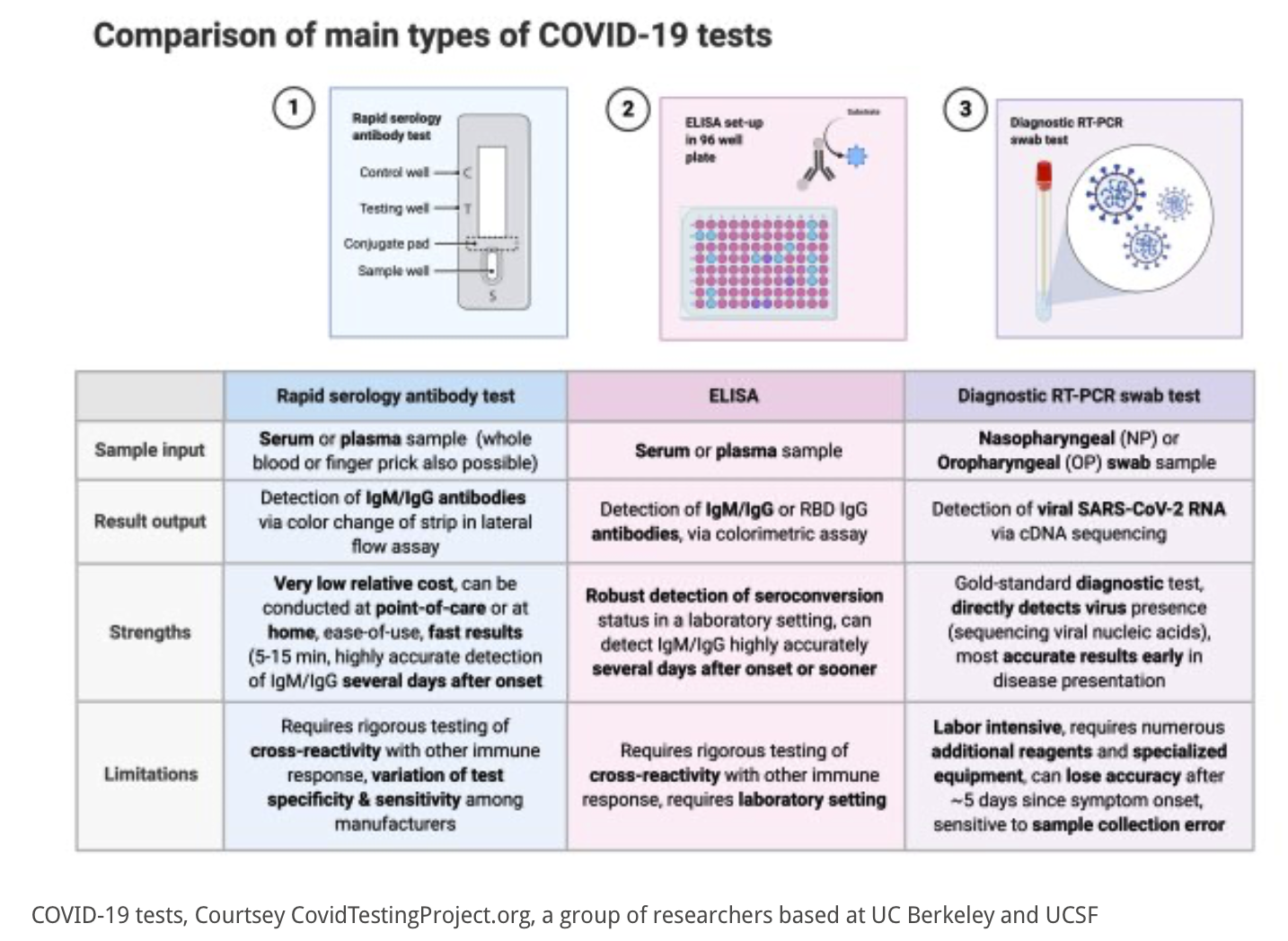
- COVID-19 ELISA IgG Antibody Test detects antibodies in the blood. If IgG antibodies are found, the lab will run a second test on the same specimen to calculate the amount of antibodies / strength of immune response (a titer).
Who should get an antibody test?
- Individuals who have previously been exposed to or are recovering from COVID-19 (based on signs and symptoms, suspected cases do not have to be laboratory confirmed).
What do these results mean for me?
- Positive results mean the patient built an immune response from their COVID-19 infection. However, in the present moment it is unknown how long these antibodies last.
- Seropositive individuals should continue to take all safety and social distancing precautions.
- It is possible that persons with antibodies can still spread the infection. There is minimal research available to confirm whether or not seropositive individuals are safe from transmitting SARS-CoV-2.
How do I donate?
The blood bank will contact individuals with positive antibody test results for donation opportunities. Please go to nybloodcenter.org for more information.
For family members who wish to donate, please complete this survey. Once completing the survey, a research staff will reach out if/when the family member is eligible.
Who receives my test results?
- Mount Sinai health care provider, the Blood Bank, Department of Health, and the FDA.
Who is eligible for antibody treatment (The FDA’s Convalescent Plasma Expanded Access Program (EAP))?
-
Inclusion criteria includes, but is not limited to, (COVID-19 Antibody program - MSH):
- 18+ years of age
- lab confirmed COVID-19 by SARS-CoV-2 RT-PCR
- severe of life threatening COVID-19 or at risk of such an infection (dyspnea, respiratory frequency >30/min, O2 saturation of less than 93%, septic shock, multiple organ failure or dysfunction, etc)
- patient or proxy able to provide consent
-
Contraindications:
- Known hypersensitivity to immunoglobulin
- Known IgA deficiency
- Discuss with Transfusion Medicine for case-by-case evaluation.
- Be cautious for individuals with end-stage renal disease or with hypercoagulability/history of hypercoagulability.
Different Types of COVID-19 Testing